Celebrity urologist tells the truth about prostate cancer
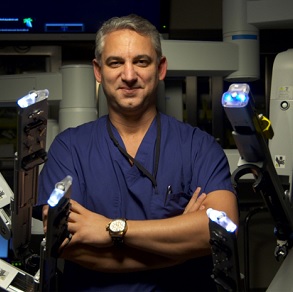
There is something that affects millions of men every year and that’s prostate cancer. Urologist dr. David Samadi is one of the most qualified professionals to answer simple questions like how do you detect prostate cancer, what can you do to watch for it and what do you do if you receive a prostate cancer diagnosis. The most important fact that people need to know is that, in 2016, 30.000 men died from prostate cancer. The disease is highly curable if caught early on and experienced surgeons like dr. Samadi play an important part in raising general awareness on the issue.
First of all, how do you know you have prostate cancer? What are the symptoms?
Dr. Samadi: The answer is that it’s asymptomatic – you should absolutely have no symptoms. That’s why they call this disease a silent killer. It’s important for you to go to the doctor, get your PSA, know what your numbers are and look at the trend. At the same time, urologists will examine your prostate and 15% of the time they may feel a nodule.
What does a prostate nodule feel like?
Dr. Samadi: Your prostate typically would feel very soft and smooth like the palm of your hand. If it feels like a knuckle and it’s firm, that’s a problem. We will get an MRI fusion biopsy in our center at Lenox Hill Hospital in New York and ensure a precise diagnosis of prostate cancer, if that is the case.
What is a PSA number and why is it so important?

Dr. Samadi: First of all, you should know that the Prostate Specific Antigen is not a specific protein for prostate cancer. It just shows you that there’s something going on in the prostate. You go to the doctor, you get a blood test and you get the PSA number. You’ve got to follow it like a stock market chart. When you have a PSA over 4, only 30% of the time it’s prostate cancer. What else could it be? For example, an infection can cause the growth of the gland and a lot of times your urologist will prescribe antibiotic first to see if that can bring the score down before beginning to worry. Next, your doctor should try to figure out if the gland could be growing: this can be followed with a trend velocity or PSA velocity: if the numbers suddenly start to zoom up, then there may be cause for worry. Everything should be done in conjunction with a digital rectal exam, where we’re feeling for a nodule and follow up with a PSA.
A lot of men don’t like the idea of the old-fashioned method of inspecting the prostate. Are there other ways except the digital rectal exam to look for prostate cancer?
Dr. Samadi: I think it’s interesting that you bring this up, because today we can get a lot of genetic tests that we have in our practice at Lenox Hill. We have urine tests called PCA3 and also we have MRI imaging studies. The MRI studies mean that we take the pictures of the ultrasound and make a fusion with the images and, just like a GPS, it will find what area in your prostate is more susceptible and more prone to get prostate cancer. This will allow for a more specific course of action.
So let’s say you’re diagnosed with prostate cancer. What do you do now?
Dr. Samadi: We’ve seen a lot of ads about radiation and surgery. The certain fact is that the one-size-fits-all is the wrong medical approach. You have to talk to your urologist about what would be the best option for treating your prostate cancer. What I like about surgery is the fact that, a lot of times, you remove the prostate and surgery is the only practice that gives you a very accurate staging. How much cancer you have, tracking changes in your PSA after surgery. The value should be zero and undetectable so you can rest at night. This is not the same with radiation. If somebody will get surgery first and the cancer comes back, you can try radiation. Meanwhile, after radiation, if the cancer comes back, in most cases, you can’t get surgery. After the prostate is removed, we follow the PSA and as long as it’s undetectable you’re cured.
My PSA has almost doubled to a 3.8, in a few years. Should I be worried?

Dr. Samadi: I say no and I’ll tell you why. Assuming that your prostate exam is normal, the digital rectal doesn’t surface any bumps, any ridges, I wouldn’t worry, because the magic number is 4. The slight increase you’re seeing is equal to getting a little bit older and your prostate’s getting a little bit bigger. But if you’re below four, I can tell you there’s an 85% chance that you do not have prostate cancer. This is why keeping a track on your PSA can be reassuring.
People should get their PSA at the age of 40 especially if they have a family history of prostate cancer. They should know ahead of time. If it’s over 1.5 at the age of 40, that’s a big red flag. The number 4 is not always the benchmark. A major factor is how big your prostate is, because you may have an 80 gram prostate and that’s why your PSA would be higher than someone whose prostate would be 60 grams. The size of your prostate has something to do with the PSA as well. Have you had any infections recently, do you have any inflammations or prostatitis? These are all extremely important and the bottom line is, if you’re diagnosed with prostate cancer there are some low-risk ones that we can just observe, as long as it’s contained.
Should I go to a specialist or a urologist for my PSA?
Dr. Samadi: I want to give a word of caution on that, these days, sometimes internists do too much. Yes you can go to one and be screened, but if there’s something wrong he or she will certainly direct you to a urologist. Specialists have a role too and they should be contacted as soon as the problem falls out of the hands of the internist.
Doctor Samadi, you are chief of robotic surgery. Is that available to every place in the nation?
Dr. Samadi: That’s an excellent question! There are a lot of robots out there, but the experience and the person behind these robots is what determines your outcome. I have done well over 7,000 surgeries. We have a team, I perform the entire case, the whole Center is dedicated to prostate cancer. We have about a thousand robots out in the United States, but doctors don’t know how to use them. You want to go to a Center of Excellence, where trained doctors have done couple of thousands of these. We’re going in the direction of less invasive surgery, more minimal surgery. It makes sense the less surgery you have, the earlier you get home, the better you get back on your feet. You better make sure that the person has a lot of experience with that particular kind of surgery and, as far as the PSA is concerned, to put this all together. Once the prostate is out you shouldn’t have a PSA. It should be zero, so then surgeons can follow that to make sure there’s no come back.
For any questions that men may have regarding the disease, you can contact dr. David Samadi and set up an appointment at prostatecancer911.com.
